Current advancements in bioengineering, AI, supercomputing, and ML are reshaping the landscape of the pharmaceutical industry. They are anticipated to make an even greater impact and draw a new vision to guide pharmaceutical research and innovation in the coming years.
Rapid scientific and technological innovations have enabled us to manipulate complex living systems and expanded our understanding of human biology. Additionally, the unprecedented investment in pharmaceutical research and development, enormously increased the identification of novel targets and their associated modalities. However, drug development is still a costly undertaking that involves a high risk of failure during clinical trials. The number of new molecular entities annually approved by the Food and Drug Administration (FDA) remains low, the likelihood of success continues to fall, and the number of drug withdrawals has shown historic increase. Therefore, it is time to transform the traditional approaches of drug development to reduce the development costs and allow medicines to reach patients faster. In addition, pharmaceutical companies are facing increasing public and political pressure to reduce the prices of drugs, which may imply lower returns. In response, large investments are directed towards translational research to find innovative tools that accelerate the drug discovery and development processes. The success of one drug would stimulate reinvestment of drug sales into the development of new drugs. This innovation cycle is essentially impacted positively/negatively by the success/failure of the initial development of a drug [Saadi and White, 2014]. In fact, the impact of innovation on dug development within the pharmaceuticals industry has not been fully realised the same way in other industries [https://druginnovation.eiu.com/, The economist]. This can be attributed to three limitations factors: 1) technical constrains that is associated with lack of understanding of the underlying science; 2) financial constrains that caused by technical risk which leads drug makers to favour safer investment, hence less innovation; 3) regulatory constraints which make it difficult to approve new drugs due to uncertainty about new ways to combat disease.
Drug discovery and development processes are complex and lengthy. Progress and evolution in the way new drugs are discovered is the need of the hour; and this evolution benefits from the emergence of new technologies. Over the past few years, there have been numerous technological advancements within the pharmaceutical industry that display immense potential for expanding the boundaries of pharmaceutical research. Specifically, the integration of various (bio-)engineering disciplines, computing, and data science into the medical and pharmaceutical fields has enabled the application of engineering principles to tackle challenges in biology and medicine, leading to a new era of technological breakthroughs in the detection and manipulation of a wide spectrum of biological entities.
We are witnessing a leap in data science and technology where the intersection of data generation, automation, and supercomputing offer unprecedented advances for the pharmaceutical industry. The current drug development process is inherently sequential, and success is defined based on data, which is usually unshared, from unrepresentative models. These processes are associated with tremendous waste of resources and cost. Implementing smart technologies is anticipated to be the most impactful strategy that will revolutionise the existing drug development paradigm. In silico methods, digitalisation, AI, and ML are proposed to play an important role in the drug development cycle, from R&D stages through the clinical trials, and in commercial manufacturing. For instance, digitalisation allows connecting disparate data sets from data management systems across the whole processes which significantly enhance the workflow efficiency. Smart drug development allows design and validation early in parallelised processes and quickly identifies dead-end outcomes before investing in heavy experimentation which save costs and time. Digitalisation converts analog data to be used in complex analysis and ML,which in turn empowers the prediction capability. Moreover, this enables researchers to match the shared data from partners across the ecosystem including academia, contract research organisations (CROs), and contract development and manufacturing organisations (CDMOs) which save time and costs [Mirasol, 2023].
Unsurprisingly, Besides automation and digitalisation, AI and ML techniques are increasingly used in drug development. For instance, AI and ML can be used to generate compound hits for a given target by predicting the likelihood that a particular compound from billions of potential molecules will interact with the target in a desirable way [Olivecrona, 2017]. This is done by: 1) virtual screening of large compound libraries to identify compounds that are likely to bind to the target of interest; 2) designing new compounds based on the structural features of known ligands that are known to bind to the target; 3) designing new compounds based on the 3D structure of the target and its binding site, and 4) generating novel compounds that have not been previously synthesised or tested for their ability to interact with the target. AI and ML can develop models that can predict the mechanism of action of a compound by analysing its chemical structure and its interactions with biological targets. These models can be trained on large datasets of known compounds with known mechanisms of action to identify patterns and predict the mechanism of action of new compounds and their possible toxicity [Cholleti, 2018]. Furthermore, AI and ML techniques can be used to understand how drug candidate efficacy may vary in different patient populations by analysing large-scale patient data, such as electronic health records, clinical trial data, and genomic data [Liu et al, 2019]. In June 2021, NVIDIA launched its supercomputer to support AI and ML research in life sciences, including drug discovery and development, genomics, and medical imaging. Following the launch of Cambridge-1, NVIDIA announced a series of collaborations with pharmaceutical companies including Astrazeneca, GSK, Novartis and Oxford Nanpore to accelerate the discovery of new drugs [NVIDIA. (2020, October 21)]. Fugaku is a supercomputer developed by Fujitsu and RIKEN, a Japanese research institute in 2020 which is currently the fastest supercomputer in the world. Fugaku is equipped with AI accelerators that enable it to perform AI and ML tasks at a high level of performance. Fugaku was used extensively in COVID-19 research, including drug discovery and development, epidemiological modelling, and medical imaging analysis [Ota, 2021]. Another supercomputing power is quantum computing which can be used to simulate the behaviour of complex molecules, such as proteins and enzymes, and predict how they will interact with potential drug compounds [McArdle, S. 2021]. In September 2018, Boehringer Ingelheim launched a collaboration with Google Quantum AI to explore the potential of quantum computing in drug design and in silico modelling. The collaboration aims to leverage Google's expertise in quantum computing and Boehringer Ingelheim's expertise in drug discovery to accelerate the discovery and development of new drugs. However, it should be noted that quantum computing is still in its early stages, and there are significant technical and practical challenges that must be overcome before it can be widely adopted in drug discovery. The combination of AI and supercomputing enables the simulation of more complex molecular interactions and the analysis of larger amounts of data than either technology alone. While machine learning allows optimising the performance of supercomputing simulations and identify the most promising drug candidates for further study.
Another exciting emerging technology in healthcare is gene editing which enables the insertion, deletion, modification, or replacement of DNA in a genome. Tessera Therapeutics develops gene editing platform based on the CRISPR-Cas technology and uses a new approach called "gene writers" to edit genes. This platform involves cutting and pasting DNA in the genome and can selectively activate or deactivate genes by adding or removing small chemical tags, epigenetic modifications at specific locations in the genome [https://www.tesseratherapeutics.com/gene-writing]. Tessera has partnerships with several pharmaceutical companies, including Novartis and Biogen, to develop gene editing therapies for various diseases.
Animal models are still the gold standard for drug research to evaluate the potential efficacy and toxicity of drug candidates before they are tested in humans. In fact, most drugs entering clinical trials are tested with limited human genetic backgrounds before they are given to people. But the results obtained from animal studies may not always accurately predict their effect in humans. Animals and humans may differ in their physiology, metabolism, and immune response, which can affect how they respond to drugs. Furthermore, the use of animal models is based on the assumption that the underlying biology of the disease being studied is similar in animals and humans. However, this assumption may not always hold true, particularly for complex diseases such as cancer or neurological disorders. In December 2022, the US House of Representatives passed the FDA Modernization Act of 2022, which eliminates the animal-testing mandate for drug development and replaces this strategy with 21st-century methods that focus on Replacing, Reducing and Refining (3Rs) the use of laboratory animals through the adoption of New Alternative Methods grounded on human biology.
The infusion of bioengineering disciplines, such as biomaterials science, tissue engineering, and nanotechnology in drug discovery involves applying engineering principles and techniques in drug discovery. Tissue engineering allows scientists to move from simple single-cell models to larger multicellular structures and to explore the intra- and extracellular environment, especially the extracellular matrix (ECM) or niche.
Organoids are 3D structures composed of self-organising cells that recapitulate key features of tissues or organs in vitro. These 3D tissue models transform biology from 2D to 3D space by providing a more physiologically relevant environment for studying complex biological processes. According to Roche, human model systems like organoids could revolutionise the way data is gathered in drug development, leading to more accurate predictions of patient responses to new molecules paving the way for more effective drug discovery and development. Therefore, the company believes that it is the opportune time to invest heavily in this cutting-edge technology. This strategy represents a significant shift towards a more human-centric approach to drug development. The Swiss drugmaker has set up a new research entity, the Institute of Human Biology (IHB), in 2021. The rebranded, Basel-based institute is the new name for Roche’s Institute for Translational Bioengineering and led by Matthias Lutolf, a pioneer professor of bioengineering at the Swiss Federal Institute of Technology/Lausanne. Roche plans to grow the IHB to around 250 scientists and bioengineers to harness the organoid technology in drug discovery and development process from target identification and target validation through preclinical safety and efficacy to stratification in clinical trials. Human stem cell-derived organoids enable researchers to identify human-specific drug targets, disease mechanisms and toxicity which mice may miss. Researchers can even develop patient-specific organoids to determine the best treatment for an individual patient. Unlike iPSC-derived organoids, patient-derived organoids require no reprogramming steps of stem cells to develop in fully functional 3D tissue structures, hence, preserve the genetic characteristics of the original tissue and the pathophysiology of the patient’s disease. Organoid Technology is exponentially growing, and we have seen several companies working on developing and commercialising this technology. For instance, Hubrecht Organoid Technology has developed a platform for generating and characterising organoids from healthy and diseased tissues based on the Lgr5+ stem cells in the adult intestine by the Hans Clever´s lab [Barker et al, 2007], which subsequently led to the development of the fist “mini-gut in a dish”. Organoid Therapeutics is another biotechnology company that is focused on developing organoid-based therapies for various diseases, including cystic fibrosis and inflammatory bowel disease. Some of the exciting development is using the iPSCs to generate insulin-producing pancreatic islet cells and incorporating it in pancreatic organoids. The technology also promotes microvasculature formation within the organoids by integrating micro-vessel fragments in the 3D cellular structure, leading to the formation of a functional vascular network.
As this field continues to grow, we can expect to see more companies developing and commercialising organoid-based products and services.
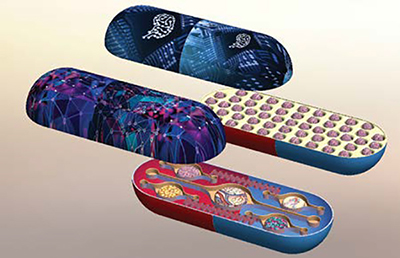
Multiple cell types/organs, originated from humans, are now being grown onto single chips demonstrating promising possibilities for assessing drug toxicity and mechanisms of action. The target of the OOC technology is to create effective and translatable integrated microphysiological models which recapitulate the key structure and functions of a specific human tissue or a network of functional organs in vitro for investigating the physiological events that characterise the interaction between organs, immune system, and exogenic substances in health and disease states. OOC devices are created by integrating microfabrication and microfluidic techniques with heterogeneous cellular structures and ECM by incorporating complex microfluidic networks that link various cell types from different organs onto a single tiny chip.
While both organoids and OOC technologies aim to mimic the architecture and function of human organs, there are key differences between them. Organoids have a relatively simple structure that can be generated from iPSCs or tissue-specific adult stem cells and are capable of self-organising into 3D structures with multiple cell types. OOCs, on the other hand, enable more complex integration of cellular/tissue components thanks to the microfluidic and microfabrication techniques which provide superior cell-cell or tissue-tissue interfacing. OOCs represent a sophisticated form of cell culture architecture that provide precise cellular positioning and in vivo-like cell polarisation by using microfabricated tailored fluidic templates on which cells can reproduce a complex assembly and mimic the actual tissue organisation. Therefore, OOC devices can provide a more physiologically relevant environment for testing drug toxicity and efficacy. Researchers are constantly developing new organ-on-a-chip using relatively similar device architecture with many attempts to integrate these devices with other techniques such as sensing and high-throughput screening. The OOC technology is still in the early stage, but its technology readiness level is increasing rapidly due to the considerable interest among researchers in academia and industry. In recent years, a number of start-ups have introduced devices or tools based on OOC technology for in vitro modelling. Of these products, the OrganoPlate® platform by MIMETAS has demonstrated a wide range of applications. TissUse GmbH (Berlin, Germany) introduced a variety of HUMIMIC Chips for different in vitro modelling purposes. The organ models are connected by microfluidic channels, which are covered with human dermal microvascular endothelial cells. Emulate Inc. (Boston, USA) is currently commercialising a variety of organ chips based on the lung-on-a-chip which was developed by the Wyss Institute at Harvard University [Huh et al 2010].
Regulatory agencies, such as the FDA, are currently considering the use of OOC devices in drug development and toxicity testing. Guidelines and standards are being developed to ensure the reliability and reproducibility of data generated from these devices. Overall, OOC is a rapidly evolving field that has the potential to transform drug discovery and development. As technology continues to advance, we can expect to see more widespread adoption and commercialisation of OOC devices, as well as the development of more complex and physiologically relevant models.
Bioprinting originated from the more established 3D printing but uses bioinks (cells and gels) as printing materials. Bioprinting uses a digital file as a blueprint to print the tissue or organs using cells as a building block which involves printing cells layer by layer to create a functional tissue [Ramadan 2021]. Like 3D printing, 3D bioprinting has the ability to control cell deposition in the x, y and z axes to create tissue-specific patterns with in vivo-like architecture which exhibit tissue-like density with highly organised cellular features, including intercellular tight junctions and microvascular networks. 3D bioprinting has great capability to produce complex 3D microfluidic architectures with multi-compartment which enables growing various cell types arranged in specific, discrete positions that enhance tissue-tissue crosstalk. This approach enables the creation of complex tissue structures with highly organised cellular features that closely resemble those found in native tissues and encourage the formation of cell-cell crosstalk and signalling pathways that are critical for the proper function of tissues and organs.
The first 3D bioprinter was developed by Organovo® in 2009. Today, there are several bioprinter platforms available for tissue and organ printing, each with their own unique features and capabilities for example, NovoGen MMX Bioprinter from Organovo, BIOXTM from CELLINK, EnvisionTEC 3D-Bioplotter from 3DSMAN, Rgen200 from RegenHU, NGB-R bioprinter from Poietis and Allevi 2 from Allevi3D. In 2021, CELLINK announced a collaboration with researchers at the University of British Columbia to develop a 3D bioprinted model of a functional kidney tissue that can be used for drug testing and disease modelling. Earlier, the company developed 3D bioprinted liver, heart and skin tissue.
The FDA recognises the potential of 3D bioprinting for regenerative medicine and tissue engineering and is taking a proactive approach to regulating this technology. The agency is working to establish regulatory frameworks and guidelines to ensure that 3D bioprinted products are safe, effective, and of high quality.
Integrating these powerful technologies is expected to revolutionise the pharmaceutical industry by accelerating the drug discovery and development process, enabling the development of more effective and personalised treatments, and reducing the time and cost of bringing new drugs to market. OOCs allow testing the safety and efficacy of drugs in an accurate way and bioprinting technology allow creating customised tissues and organs that are specific to an individual patient while AI and ML can be used to analyse the data generated by these models, helping to identify potential drug candidates more quickly.
More technological advances will continue to infuse into pharmaceutical research and development, and it is exciting to see how drug discovery and development will be reshaped to make drugs more affordable for patients.
References
[1]. Saadi, E., & White, G. (2014). Rewarding Innovation in Drug Development. American Health & Drug Benefits, 7(7), 373-374. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4268767/
[2]. Feliza Mirasol, Using Smart Tools for Smart Development, Pharmaceutical Technology, Pharmaceutical Technology, May 2023, Volume 47, Issue 5, Pages: 16–20, (https://www.pharmtech.com/view/using-smart-tools-for-smart-development)
[3]. Olivecrona, M., Blaschke, T., Engkvist, O., & Chen, H. (2017). Molecular de-novo design through deep reinforcement learning. Journal of chemical information and modeling, 57(11), 2657-2668.
[4]. Cholleti, A., Varsani, A., Xia, J., & Herman, B. (2018). Machine learning for drug toxicity and efficacy prediction. Journal of chemical information and modeling, 58(4), 820-846.
[5]. Liu, Y., Wu, L., & Zhu, X. (2019). Personalized drug recommendation based on patient similarity and drug similarity. IEEE/ACM Transactions on Computational Biology and Bioinformatics.
[6]. NVIDIA. (2020, October 21). NVIDIA Launches UK's Most Powerful Supercomputer, Dedicated to AI Research in Healthcare and Life Sciences. NVIDIA Newsroom. https://nvidianews.nvidia.com/news/nvidia-launches-uks-most-powerful-supercomputer-dedicated-to-ai-research-in-healthcare-and-life-sciences.
[7]. Ota, S., Yamamoto, Y., Imai, H., & Nakamura, H. (2021). Fugaku: The Supercomputer for Fighting COVID-19. IEEE Micro, 41(2), 10-15.
[8]. https://www.tesseratherapeutics.com/gene-writing
[9]. McArdle, S. (2021). Quantum computing for the pharmaceutical industry. Drug Discovery Today, 26(1), 83-88.
[10]. Barker et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 2007, 449:1003–1007.
[11]. D. Huh, B. D. Matthews, A. Mammoto, M. Montoya-Zavala, H. Y. Hsin, and D. E. Ingber, Science 328(5986), 1662–1668 (2010).
[12]. Qasem Ramadan and Mohammed Zourob, 3D Bioprinting at the Frontier of Regenerative Medicine, Pharmaceutical, and Food Industries, Frontiers in Medical Technology, 2021, Volume 2, Article 607648